The switch from anatomopathological diagnosis to imaging diagnosis in adenomyosis
Image Description
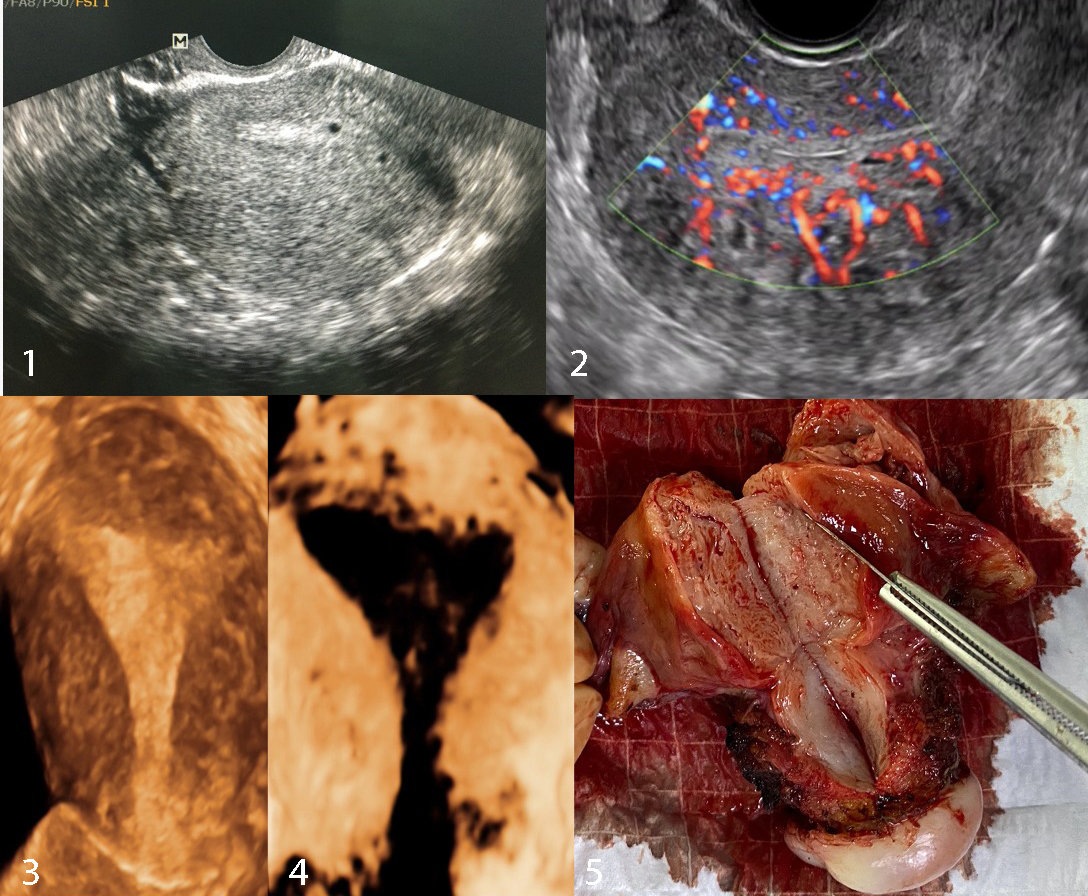
Adenomyosis is defined by the inappropriate proliferation of the endometrial glandular and stromal tissue within the smooth muscle of the uterine myometrium. The symptoms and signs vary widely, but the most common are dysmenorrhea and/or chronic pelvic pain and menorrhagia. It was classically described as a multiparous, pre-menopausal disease in women in their thirties to forties, but the improvement of the diagnostic ability of ultrasound and MRI shed more light on the affected population (Fig 1.). Therefore, more cases of adenomyosis in women under thirties have been described lately [1].
Color Doppler is an efficient imaging modality to demonstrate increased tortuous vessels throughout the myometrium (Fig 2). The 3D ultrasound technology has recently helped establish stronger criteria for diagnosing adenomyosis, allowing to assess of the lateral and fundal aspects of the Junctional Zone (JZ) and providing a sharper visualization of the endometrial protrusions in the uterine wall (Fig 3), (Fig.4) [2]. The Junctional Zone is the endo-myometrial junction, that identifies a functionally and structurally different tissue from the myometrium [3]. The most specific parameters in 3D-transvaginal ultrasonography are JZmax>8mm, hypoechoic striation, and myometrial asymmetry [4]. The levonorgestrel-releasing intrauterine device (LNG-IUD) is a successful treatment option, but the hysterectomy or the focal excision is the definitive cure when the disease is refractory to medical treatment (Fig 5) [5].
References
. Gunther R, Walker C. Adenomyosis. 2021 Jul 22. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan–. PMID: 30969690.
. Chapron C, Vannuccini S, Santulli P, Abrão MS, Carmona F, Fraser IS, Gordts S, Guo SW, Just PA, Noël JC, Pistofidis G, Van den Bosch T, Petraglia F. Diagnosing adenomyosis: an integrated clinical and imaging approach. Hum Reprod Update. 2020 Apr 15;26(3):392-411. doi: 10.1093/humupd/dmz049. PMID: 32097456.
Luciano DE, Exacoustos C, Albrecht L, LaMonica R, Proffer A, Zupi E, Luciano AA. Three-dimensional ultrasound in diagnosis of adenomyosis: histologic correlation with ultrasound targeted biopsies of the uterus. J Minim Invasive Gynecol. 2013 Nov-Dec;20(6):803-10. doi: 10.1016/j.jmig.2013.05.002. PMID: 24183272.
. Brosens JJ, de Souza NM, Barker FG. Uterine junctional zone: function and disease. Lancet. 1995 26;346:558–560.
Abbott JA. Adenomyosis and Abnormal Uterine Bleeding (AUB-A)-Pathogenesis, diagnosis, and management. Best Pract Res Clin Obstet Gynaecol. 2017 Apr;40:68-81. doi: 10.1016/j.bpobgyn.2016.09.006. Epub 2016 Sep 30. PMID: 27810281.