Multidisciplinary management of a gastric fistula after laparoscopic sleeve gastrectomy
Image Description
We present the case of a 23-year-old patient with a BMI of 42 kg / m², hypertension and gonarthrosis who presented for an evaluation regarding bariatric surgery. After the preoperative investigations and consults were obtained a laparoscopic sleeve gastrectomy was done. The first two postoperative days were uneventful but on day 3 the patient became tachycardic, febrile and purulent fluid was observed on the perigastric drain. An abdominal CT was obtained which confirmed the diagnosis of a gastric fistula. Reintervention was undertaken with primary laparoscopic suture of the gastric fistula, peritoneal lavage, and drainage. Three days after the second surgery the gastric fistula re-opened. After interdisciplinary evaluation, a conservation tactic was decided upon and an expandable gastric stent was mounted via an upper endoscopy. Seven days after, the stent migrated towards the duodenum so a second stent was mounted. The evolution after the second stent was favourable, the drainage tube was extracted 7 days and the gastric stents were extracted at 1month. One year after the surgery the patient showed a favourable evolution with considerable weight loss. Post-surgical complications in gastric-sleeve patients warrant extreme care and multidisciplinary management ensures optimal results.
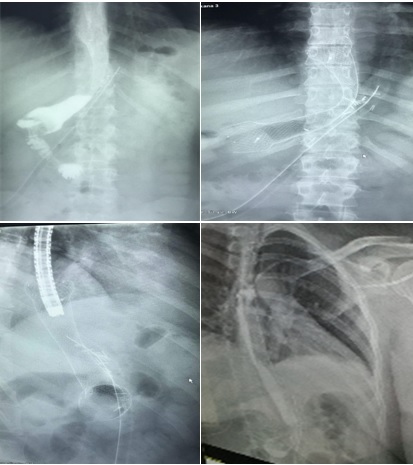
The first picture on the left identifies the gastric fistula with a barium X-ray, the following pictures (2, 3) describe the process of mounting the stent under x-ray guidance and figure 4 demonstrates gastric contention of the barium after the stent was mounted.