Cutaneous leukocytoclastic vasculitis
Image Description
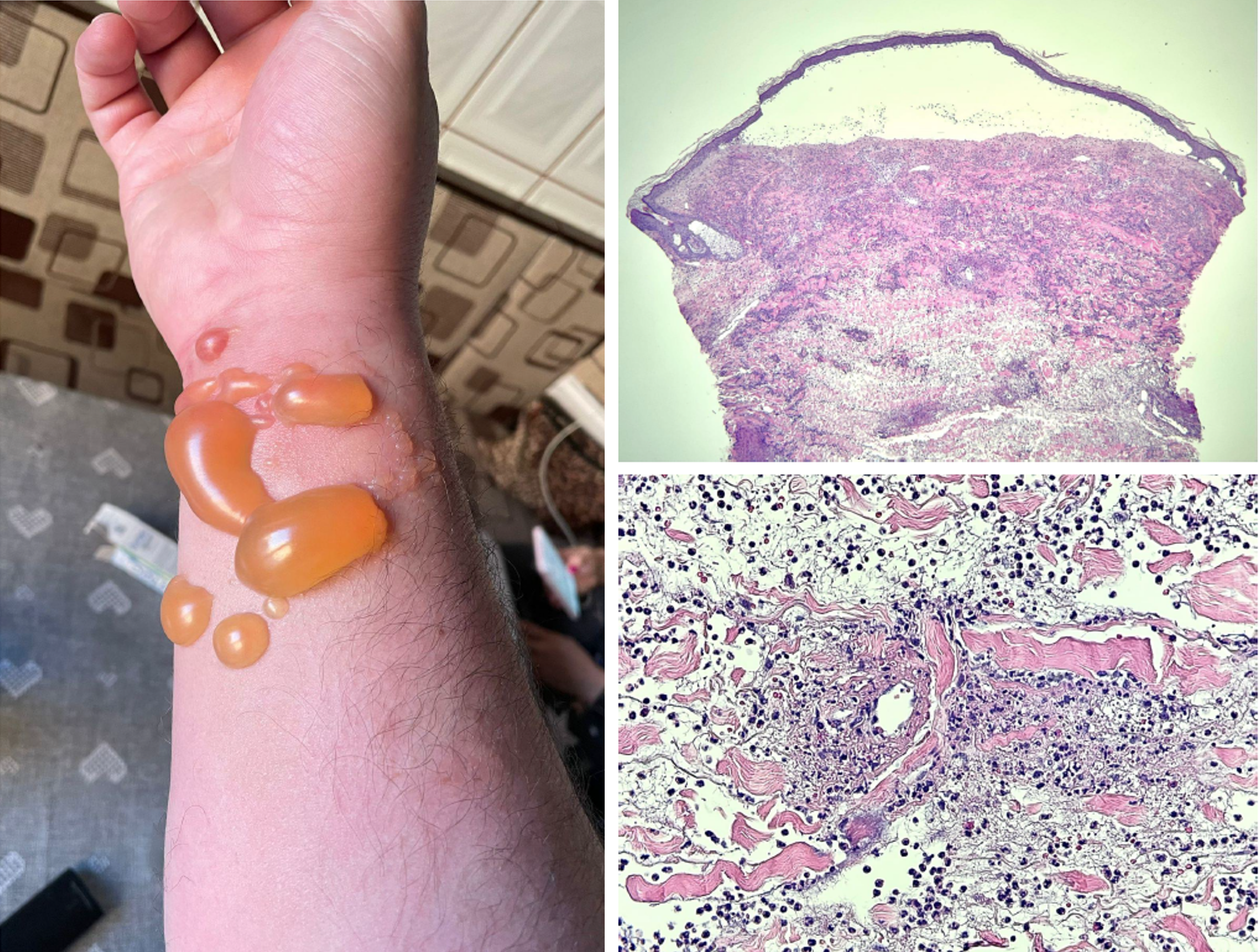
Cutaneous leukocytoclastic vasculitis (LcV) represents a skin disorder, a distinct form of vasculitis affecting one organ. It can also be a component of systemic vasculitis. Vasculitis symptoms vary by blood vessel size, location, and depth. Urticarial plaques, papules, and palpable purpura result from superficial small vessel involvement. Increased penetration at the dermohypodermic junction or hypodermis may cause ulcers, nodules, or livedo. Diagnostics depend on the type of infiltration, as LcV is a common histologic feature rather than a separate disease entity.(1) Our case of a 48-year-old man with atypical LcV highlights the importance of clinical observations and histological and immunofluorescence results. The patient had extensive, itchy skin rashes that developed over two years. It appeared as transient erythematous plaques and tense bullae on the forearms and posterior thigh. A comprehensive test battery, including serological and allergen-specific IgE measurements, unveiled sensitivities to analgesics and fragrance components.. LcV was diagnosed by 26 hours following the onset of symptomatology and paired with histopathological and direct immunofluorescence findings. The neutrophilic and lymphocytic infiltrate with fibrinoid necrosis and deposits of IgG, IgM, and complement components in the cutaneous vasculature were present. During the differential diagnosis, Sweet syndrome and hypersensitivity reactions were considered due to their similar clinical and histopathological features. Absence of BP180 and BP230 autoantibodies ruled out bullous pemphigoid in this patient. (3,4)
This patient's bullae are unusual for LcV. Even after extensive testing, the cause was unknown, supporting idiopathic nature. Clinical improvement occurred after dapsone, which modulates neutrophil function, was introduced.
References
Frumholtz L, Laurent-Roussel S, Lipsker D, Terrier B. Cutaneous Vasculitis: Review on Diagnosis and Clinicopathologic Correlations. Clin Rev Allergy Immunol. 2021;61(2):181-193. doi:10.1007/s12016-020-08788-4
Fraticelli P, Benfaremo D, Gabrielli A. Diagnosis and management of leukocytoclastic vasculitis. Intern Emerg Med. 2021;16(4):831-841. doi:10.1007/s11739-021-02688-x
Vashisht P, Goyal A, Hearth Holmes MP. Sweet Syndrome. [Updated 2022 Sep 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431050/
Baigrie D, Goyal A, Crane JS. Leukocytoclastic Vasculitis. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482159/