Myometrial arteriovenous malformation after caesarean section - case report
Image Description
Uterine arteriovenous malformations (AVMs) are an uncommon cause of vaginal bleeding (1,2). The incidence is 4.5%, however this is probably underreported (3). It is an important diagnosis to consider in women with unexplained heavy vaginal bleeding with a recent history of pregnancy (surgical abortion or cesarean section).
Acquired uterine AVMs consist of one or more arteriovenous fistulas between the intramural arterial branches and the myometrial venous plexus (4). Many uterine arteriovenous malformations evolve favorably and resolve spontaneously with conservative treatment. The predictive factors are lower-velocity flow within the AVM (PSV < 40 cm/s) and normal initial hemoglobin (4,5).
This case report describes a 35-year-old woman who presented heavy vaginal bleeding 6 weeks after cesarean section.
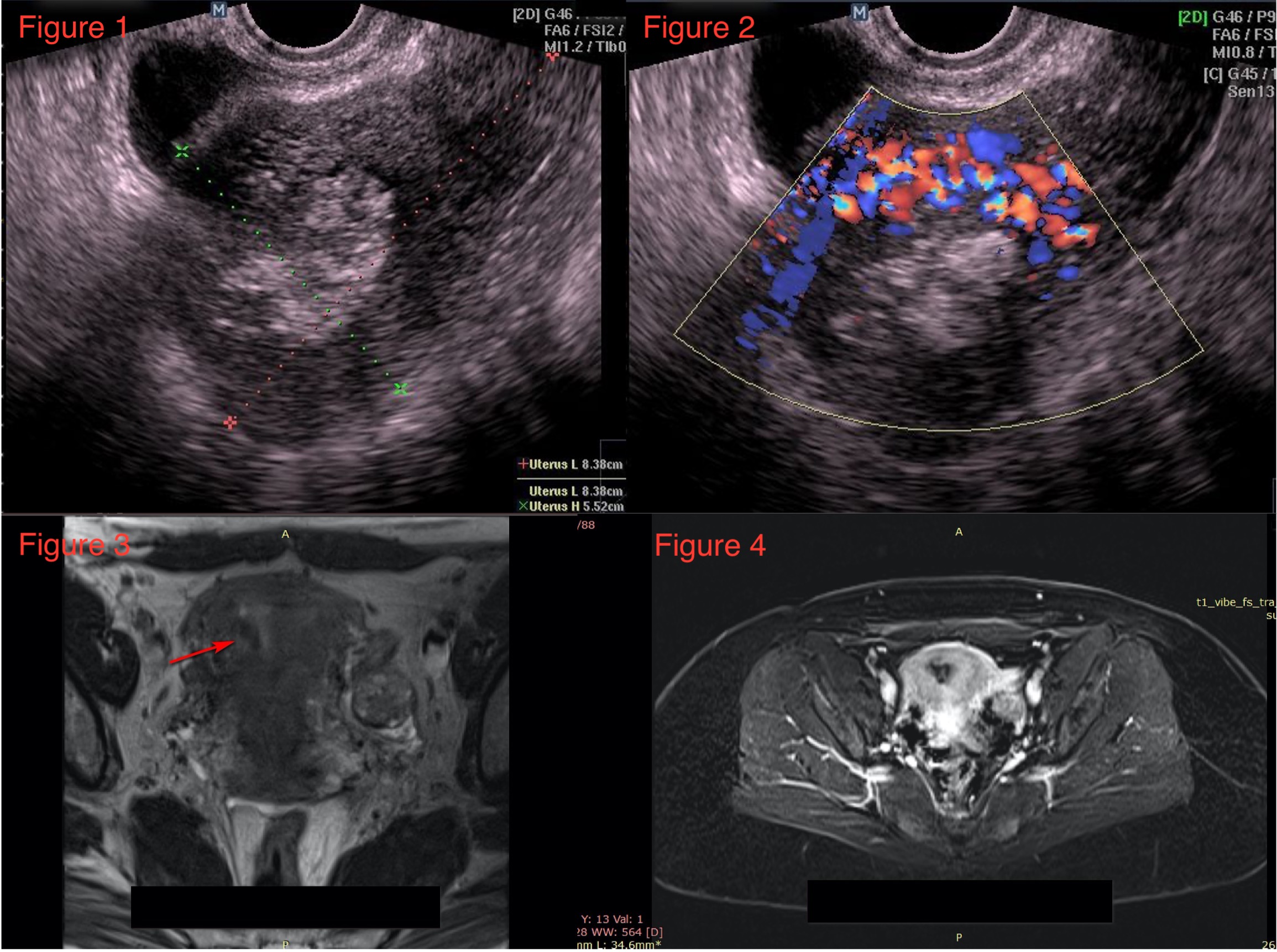
Transvaginal imaging revealed a focal, irregular, hyperechogenic area into the anterior myometrium measuring 36/40 mm (Figure 1). Spectral Doppler ultrasound (Figure 2) revealed abnormal vessels, tubular anechoic spaces, turbulent arterial and venous flow, with peak systolic velocities (PSV - 41 cm/s) and low-resistance (RI - 0.25). Serum bHCG was negative, the hemogram test showed mild anemia (Hb level of 10.2 g/dL). Ultrasound and clinical findings support the diagnosis of acquired uterine arteriovenous malformation.
Pelvic MRI confirmed the diagnosis (Figure 3,4). Multiple serpentine flow-related signal voids are seen in the anterior uterine wall, endometrial cavity, and parametrium on T1 and T2 weighted images.
The patient received a conservative treatment with gonadotropin-releasing hormone agonists for 6 months. Follow-up ultrasound showed almost complete AVM involution.
References
Radswiki, T., Bell, D. Uterine arteriovenous malformation. Reference article, Radiopaedia.org. (accessed on 09 Jan 2022) https://doi.org/10.53347/rID-14643
Gallagher N, Cincotta M, Keblawi H, Jude D, Korona M. Uterine arteriovenous malformation leading to postpartum hemorrhage: A case report. Case Rep Womens Health. 2020 Oct 3;28:e00260. doi: 10.1016/j.crwh.2020.e00260. PMID: 33088725; PMCID: PMC75O'brien P.,
Neyastani A., Buckley A.R., Chang S.D., Legiehn G.M. Uterine arteriovenous malformations: from diagnosis to treatment. J Ultrasound Med. 2006;25(11):1387–1392. 59227.
Sridhar, D.S., & Vogelzang, R.L. (2018). Diagnosis and Treatment of Uterine and Pelvic Arteriovenous Malformations.
Lee TY, Kim SH, Lee HJ, et al. Ultrasonographic indications for conservative treatment in pregnancy-related uterine arteriovenous malformations. Acta Radiol. 2014;55:1145-1152.